The International Association for the Study of Pain (IASP) defines pain as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage". Two significant types of pain are physiological (acute) and clinical (chronic). Acute pain is a normal physiological reaction to an injury that provides an early warning system that an injury has occurred, and it can help diagnose a problem (e.g., sprain/strain). Without pain, you might seriously hurt yourself without knowing it, or you might not realize you have a medical problem that needs treatment. It does not last very long, as most injuries will generally heal within three months. Chronic pain is a pain that does not go away after three months. It can be intermittent (occurring on and off) and may vary in intensity during the day, or it can be persistent. Chronic pain can result from a known cause, such as surgery or inflamed joints, or a consequence of a disease process, such as rheumatoid arthritis. Before a diagnosis is made for chronic pain, tests may be done to rule out or identify other conditions that can cause pain. These tests may include a neurological exam, orthopedic tests, and a mental health assessment. In most cases, test results are normal, making it difficult to know the exact cause of the pain due to the unknown etiology (original cause). Chronic pain can be defined as an abnormal processing of pain where the original injury or cause of acute pain has resolved, but the warning system has failed to shut off. When this occurs, the warning bells are still going off; however, they no longer signal “danger” or “harm” but indicate a pain-processing problem. There are different types of chronic pain. Two of the significant, non-cancer chronic pains are:
Musculoskeletal Pain affects the bones, muscles, ligaments, and tendons. It can result from various causes, including sports or occupational injuries, motor vehicle collisions, repetitive strain injuries, and disease processes, such as arthritis.
Neuropathic Pain: that is a complex, multi-faceted state of chronic pain with no apparent cause. It can involve damaged tissue, injury, or malfunctioning nerve fibers or changes in brain processing. An example of neuropathic pain is phantom limb syndrome. The brain still receives signals from nerves that originally carried impulses from the now missing limb. Other types of neuropathic pain include numbness, burning, "pins and needles" sensations, and shooting pain.
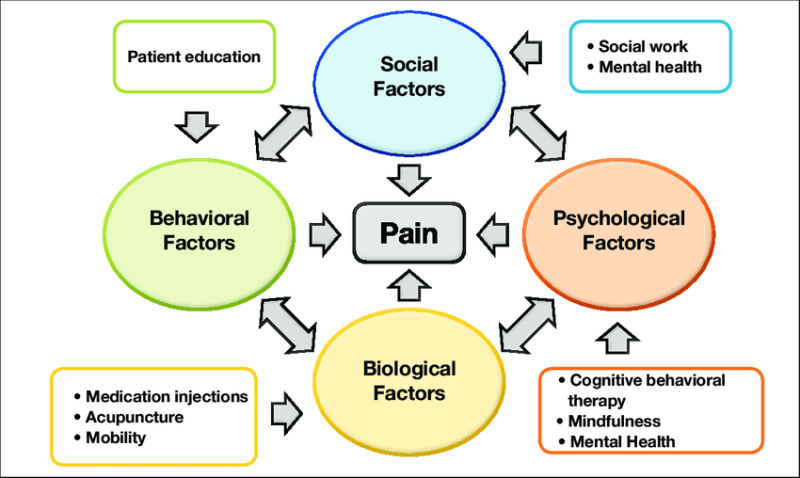
The concept of access to pain management as a human right has gained increasing currency in recent years. The United Nations and regional human rights bodies have accepted the idea and incorporated it into key human rights reports, reviews, and standards. Mild intermittent chronic pain can be treated with drugless, non-invasive methods. Regular exercise, using correct body posture/body mechanics, getting enough sleep, eating a healthy diet, and trying complementary therapies (i.e., chiropractic manual therapies, acupuncture-acupressure, massage, yoga, etc.) may help reduce chronic pain by increasing the level of the body's Endorphins. In addition, psychological counseling may help the patient cope with the pain and with common reactions they might have to it, such as frustration, fear, anger, depression, and anxiety. Chronic pain often can be successfully managed so that the patient's quality of life significantly improves; however, if the pain persists or becomes more severe, then there is a need for more invasive methods such as spinal cord stimulation, injection of local anesthetics, and pharmacotherapy with potent anti-inflammatory and/or analgesic (pain-relieving) medications. The best approach for chronic pain management is based on the Bio-Psycho-Social (BPS) model of care. In the BPS model, assessments and treatments of patients are performed by a multidisciplinary team of healthcare providers addressing the range of chronic pain's physical, psychological, and social components. Usually, the interdisciplinary team comprises medical pain specialists (MDs specialized in pain management or anesthesiologists with a fellowship in pain management), DCs, and/or Physical Therapists, Occupational Therapists, Psychotherapists, and Licensed Social Workers. The patient section of the Practical Pain Management (PPM) website provides very useful information about effective treatments and self-management techniques to increase functionality of patients suffering from chronic pain. Veritas Publication's Pain Management page offers unbiased, high-quality resources for patient education, empowering people to make informed health decisions.